|
Bladder
cancer
Bladder cancer is a relatively common disease. The major risk factor is cigarette
smoking but a number of chemicals can also produce the disease. Like many cancers
there is considerable variation in the potency of the disease and this of course
has consequences for what the disease will mean to the patient.
The
usual method of discovery of bladder cancer is by blood in the urine
(bladder cancer is only one of the causes of blood in the urine).
Early diagnosis may well catch the disease at an early stage.
When
considering bladder cancer there are two important factors to understand
in order to make predictions regarding the management of the disease
and the outcome of the disease for the patient. These are grade and
stage. I will explain these one at a time.
Grade
This is a measure of the potency of the cancer. The cancer is classified into
three grades, 1, 2 and 3. Grade one is the mildest. It is highly unlikely
that the patient will ever need major surgery of that the disease might
be lethal. Grade three is at the other end of the spectrum, this disease
must be brought under control if possible as it might spread from the bladder
and become incurable. This can be attempted with telescopic surgery at
first but in some cases where this fails to gain control more radical treatment
like radiotherapy or the bladder may even need to be removed by surgery.
Grade 2 disease is of course somewhere between the two.
The
second concept that needs to be understood is stage. This is a measure
of how far the cancer has spread into or beyond the bladder. This
again gives the surgeon information on the behavior of the patient’s
disease.
Patient
Health
Just like the management of prostate cancer it is important to take account
of the overall health of the patient. Many of our patients have been lifelong
smokers, this has usually had an impact on their lungs and heart as well as
their bladders. We therefore attempt to balance the risks of the treatment
with the patient general health.
First Steps
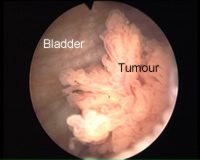
Once the diagnosis has been made the patient will be admitted to hospital for
removal of the tumour telescopically. This is performed under a general
or spinal anaesthetic (rather like an epidural). The surgeon will attempt
to remove the entire tumour. All of the tissue removed will be sent to
the laboratory to be examined under the microscope. This will provide the
information needed on stage and grade. At the end of the procedure you
will be examined again to assess rather a significant amount of tumour
has been left behind. Click here to see a short video of the procedure
(RealVideo approx. 50 seconds to download).
Patients are in
hospital for up to 24 hours after the procedure. It is normal to
see blood in the urine on and off for up to 2 weeks after surgery.
It is also common to have some burning when passing urine as well
as an ache in the lower part of the abdomen toward the end of passing.
The area where the growth has been removed is raw, rather like a
mouth ulcer. If symptoms persist for more than a week it may represent
a urinary tract infection and further advice should be sought.
A further out-patient
visit may well be arranged to make a plan based on the results of
the surgery and the stage and grade of the bladder tissue. Some surgeons
however make this plan when they receive the results of the laboratory
tests, then writing to patients rather than bringing everyone back
to the hospital.
At this point there
are a number of possible outcomes;
- A further bladder
check in 6 to 12 weeks. This is to assess whether the tumour has
been completely removed or if new growths have occurred. This is
the commonest outcome.
- The patient
may be booked for a series of chemical treatments to the bladder.
These aim to reduce the chances of the tumour coming back or invading
deeper into the bladder.
- Further tests
like body (CT) scans or bone scans may be arranged to plan for
more serious treatment (radiotherapy or major bladder surgery)
What can
I do to reduce the risk of further bladder growths?
The most important step is to stop smoking. Just cutting down is not enough.
Your GP may well be able to help you through local groups to quit. The toxins
that are inhaled during cigarette smoking pass into the body through the lungs
before many are removed from the body in the urine. Its not surprising therefore
that the commonest sites of cigarette related cancers are the lung and bladder.
Stopping reduces the risk of further cancers, it also makes major surgery much
less risky should this be needed in the future.
What happens
to most people?
Most patients end up on routine bladder check programmes. Initially the bladder
is checked three monthly, eventually yearly. In many cases patients will be
discharged after 5 to 10 years. Because of the benign nature of the disease
in many patients bladder cancer was for many years described as bladder warts
by many surgeons.
What’s
the worst that could happen?
Bladder cancer can be a serious and progressive disease. In patients who have
grade 3 (the worst type) with early invasion of the bladder more radical (extensive)
treatment is used to attempt to remove the cancer before it has spread and
cannot be cured. Depending on a number of factors radiotherapy, bladder removal
or both may be discussed.
Bladder
removal
This represents major surgery. If the bladder is removed obviously the urine
needs to be collected somewhere. The traditional method of achieving this is
via a bag worn on the abdomen. A length of bowel is used to bring the urine
form the kidneys to the surface of the body. This operation in known as cystectomy
and ileal conduit. Newer techniques may be suitable for some patients however.
It is possible using a number of new operations to create a new bladder within
the body. Patients therefore pass their water almost the way that nature intended.
There are a number of drawbacks however. It takes longer to regain control
of continence. Although a bag on the abdomen is something all of us wish to
avoid, the vast majority of people are able to return to normal activities
very speedily. Patients who have had new bladder fashioned may take up to a
year and a half to be able to stop worrying that they may leak and indeed some
people will leak for ever. In addition a small number of people with new bladders
will find that they cannot pass water unaided (particularly the case for women).
These patients will need to pass a catheter into the bladder to empty it for
the rest of their life. Why with these possible drawbacks do people opt for
new bladders? In countries such as Switzerland where the procedure is very
common about 50% of people opt for a new bladder. The commonest reason sited
for this is to avoid the need for a bag on the abdomen.
How
risky is bladder removal?
In the 1970’s as many as 1 in 10 patients undergoing this type of surgery
would die from complications. These days in most hospitals the risk is less
than 1 in 50. This is predominantly due not to advances in surgery but in post-operative
care, for example the provision of high dependency or intensive care beds.
The risk for an individual may however be higher, depending of course on other
medical problems such as angina, high blood pressure or chest problems.
These risks have
to be balanced against the risk of not having treatment. In patients
where bladder removal is indicated the risk of death from bladder
cancer without radical treatment is approaching 100%.
Alternatives
to surgery
Many patients who are considered for bladder removal are also suitable for
radiotherapy. There are a number of technical reasons why one may be more suitable
for individual patients that I will not elaborate on here. The overall success
for radiotherapy in selected patients is the same as surgery. It would be a
mistake though to believe that radiotherapy is an easier option. Treatment
consists usually of 30 treatments over the course of 6 weeks. Radiotherapy
has its own side effects such as increased frequency of passing water and diarrhoea
both of which may be permanent. In addition radiotherapy clears approximately
half of the tumours that it is used for. In those unfortunate patients who
suffer a relapse, surgery may well be required. Removing the bladder after
radiotherapy is in most surgeons experience a more difficult and risky procedure.
Additional
Treatments – Chemotherapy
Intravenous or injected chemotherapy cannot be used alone to cure bladder cancer.
It is used however in combination with other treatments such as surgery. Depending
on the specific indications in can be given prior to surgery to make surgery
possible or after surgery in a belt and braces type approach. This type of
intravenous chemotherapy should not be confused with the much more common chemotherapy
that is placed only within the bladder as a washout to decrease the chance
of bladder cancer recurring.
A Final
Point
Just to re-iterate, most patients who have a diagnosis of bladder cancer never
suffer serious harm to their health. In those who have more serious forms of
the disease prompt action saves many lives. Even after major surgery it is
possible to live a full and rewarding life. In those that have to have their
bladder removed there are nowadays often alternatives to wearing a bag on the
abdomen. And very finally, if at all possible stop smoking!
|